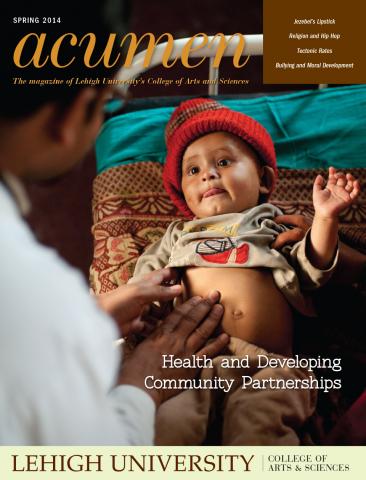
Health care professionals learn that some categories of people are more likely than others to manifest specific symptoms and diseases. Psychologist Gordon Moskowitz has been studying whether, in addition to these medically correct inferences that are made about patients, stereotypes unconsciously influence the thinking and behavior of physicians. His research finds that health care workers unknowingly categorize people according to social stereotypes and that this unconscious bias among health care workers can influence diagnoses and treatments.
In research, funded by the National Institutes of Health’s Minority Health and Health Disparities division, Moskowitz, professor and chair of psychology, and Dr. Jeff Stone, at the University of Arizona, study issues surrounding health disparities and the degree to which bias might be contributing.
In a recent series of experiments, the team asked participants to complete an experiment individually on a computer. Participants were asked to identify whether words that were to appear on the screen were names of diseases or treatments, or not, by pressing buttons marked yes or no on the keyboard. Some of the words are stereotypic words associated with a group (noncompliant-Hispanic; criminal-Black). They were asked to respond as quickly and accurately as possible. Prior to each word, and unbeknownst to the participants, the researchers flashed on the screen faces of different racial groups and flashed them so quickly subjects could not see them. Health care professionals’ responses to the stereotypic words, as well as the words related to group-relevant diseases, were different when they first “saw” a face of the relevant minority group instead of a white face.
Although doctors often use medical stereotypes and are fully aware of the positive consequences of such conscious thoughts (making appropriate diagnoses), they may also be activating unintended consequences associated with unconscious stereotyping that seemingly occurs every time they have any thought of a patient’s social group, Moskowitz says. The team found that stereotypes were triggered by subliminal cues, of which doctors could not possibly be aware, and a better understanding of bias may help in physician training.
“In the end, what can we do to prevent this from happening?” he says. “What can we do about stereotype control, and what do we know about controlling these unconscious thoughts and feelings that we can then develop effective training programs where we teach physicians how to interact with patients in ways that don’t trigger these stereotypes and have these consequences?”